What is Sickle Cell Disease: Causes, Symptoms, and Treatments
- Rosemary Britts

- Jan 1
- 14 min read
Updated: 6 days ago
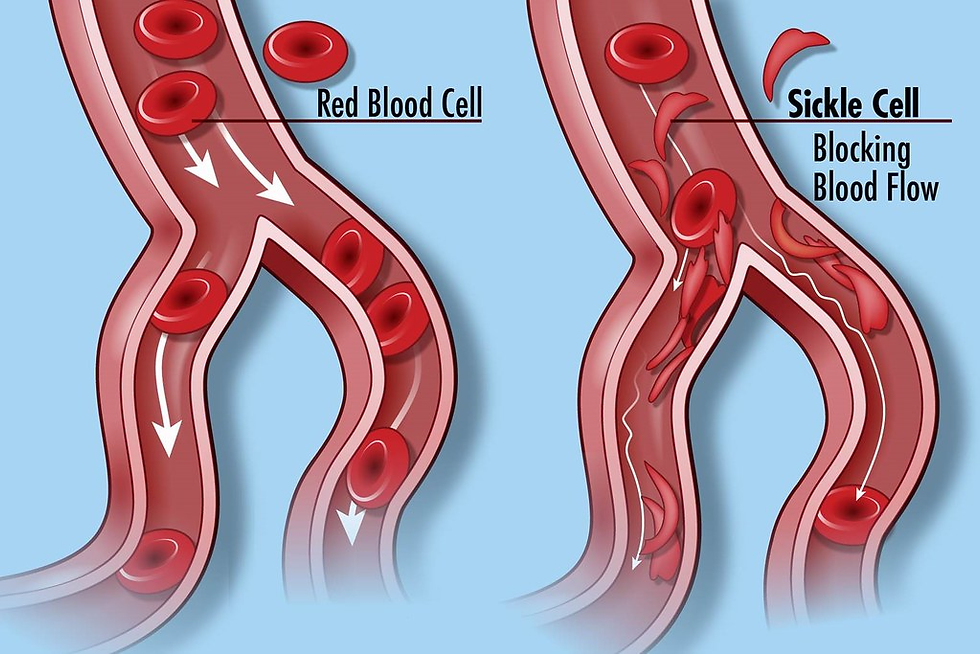
So, what exactly is sickle cell disease? It's a genetic condition that affects red blood cells, the ones that carry oxygen all around your body. Normally, these cells are round and flexible, but with sickle cell disease, they can become stiff and shaped like a sickle or a crescent moon. This can cause them to get stuck in small blood vessels, leading to all sorts of problems. It's a lifelong condition that many people live with, and understanding it is the first step.
Key Takeaways
Sickle cell disease is a genetic disorder where red blood cells become misshapen, like a sickle, instead of round.
This abnormal shape makes it hard for cells to move smoothly through blood vessels, causing blockages.
The main cause is a change in the gene that makes hemoglobin, the protein that carries oxygen.
Symptoms can include pain episodes, fatigue, and anemia, and can vary in severity.
While there's no universal cure, treatments focus on managing symptoms, preventing complications, and improving quality of life.
Understanding What Is Sickle Cell Disease
What Sickle Cell Disease Is
Sickle cell disease, often called SCD, is a genetic condition that affects your red blood cells. Normally, red blood cells are round and flexible, like tiny donuts, and they move easily through all your blood vessels to deliver oxygen everywhere your body needs it. But with sickle cell disease, something changes in the protein inside these cells, called hemoglobin. Instead of being round, the red blood cells can become stiff and shaped like a crescent moon, or a sickle. These sickle-shaped cells can get stuck in small blood vessels, blocking blood flow. This blockage is what causes a lot of the problems associated with SCD.
It's a condition that's passed down through families. You inherit it from your parents. It's not something you can catch from someone else. The sickle shape happens because of a change, or mutation, in the gene that tells your body how to make hemoglobin. This means the hemoglobin inside the red blood cells doesn't work quite right. It can clump together, especially when oxygen levels are low, making the cells stiff and sticky.
This condition is more common in people whose families come from certain parts of the world, like Africa, the Mediterranean, the Middle East, and India. It's thought that having sickle cell trait might have offered some protection against malaria in the past.
The Impact of Sickle Cell Disease
Living with sickle cell disease means dealing with a range of issues because of those sickle-shaped cells. The main problem is that they don't move through blood vessels as smoothly as healthy red blood cells. This can lead to blockages.
When blood flow is blocked, it can cause:
Pain: This is a really common symptom. Blockages can happen anywhere in the body, causing sudden, severe pain. People often describe it as a sharp, stabbing pain, or a deep ache.
Anemia: Sickle cells don't live as long as normal red blood cells. Normal red blood cells last about 120 days, but sickle cells can break down in as little as 10 to 20 days. This means the body doesn't have enough red blood cells to carry oxygen, leading to tiredness and weakness.
Swelling: Blockages in the small blood vessels can cause swelling, especially in the hands and feet. This is often one of the first signs seen in babies and young children with SCD.
Increased risk of infections: The spleen, an organ that helps fight infections, can be damaged by sickle cells. This makes people with SCD more likely to get serious infections.
These issues can affect a person's daily life in many ways, from how much energy they have to how often they can go to school or work. It's a lifelong condition that requires ongoing care and attention to manage symptoms and prevent complications. Learning about hemoglobinopathy helps understand the root of these issues.
The Genetic Basis of Sickle Cell Disease
Sickle cell disease (SCD) isn't something you catch like a cold; it's something you're born with. It all comes down to your genes, specifically the ones that tell your body how to make hemoglobin. Hemoglobin is that super important protein inside your red blood cells that carries oxygen all over your body. Think of it like the delivery trucks for oxygen.
Gene Mutations Causing Abnormal Hemoglobin
In SCD, there's a tiny change, a mutation, in the gene that's supposed to create normal hemoglobin. This change means the body makes an unusual type of hemoglobin, often called hemoglobin S (HbS). Instead of being soft and round like healthy red blood cells, the cells with HbS can become stiff and shaped like a crescent moon, or a sickle. This happens especially when they're not carrying much oxygen.
This change is caused by a single mistake in the DNA code. It's like a typo in a recipe that changes the final dish. This typo leads to a change in one of the building blocks of the hemoglobin protein, which then makes the whole molecule behave differently.
Inheritance Patterns of Sickle Cell Disease
So, how do you end up with this gene mutation? You inherit it from your parents. SCD follows what's called an autosomal recessive pattern. This means you need to get two copies of the mutated gene – one from your mom and one from your dad – to actually have sickle cell disease.
Two mutated genes: You have sickle cell disease.
One mutated gene and one normal gene: You have sickle cell trait. You're usually healthy but can pass the gene on.
Two normal genes: You don't have sickle cell trait or the disease.
It's important to know that if you have sickle cell trait, you generally don't have symptoms of the disease itself. However, you can still pass the gene along to your children. This is why understanding family history can be helpful. The sickle cell trait is more common in people whose ancestors came from places like Africa, the Mediterranean, the Middle East, India, and parts of South America. This is partly because having the trait offered some protection against malaria in those regions.
Types of Sickle Cell Disease
While we often talk about sickle cell disease as one thing, there are actually a few different types. They all involve the abnormal hemoglobin S, but the specific combination of genes can lead to slightly different conditions and severity. The most common type is Sickle Cell Anemia (HbSS). Others include Hemoglobin SC disease (HbSC) and Sickle Beta-Thalassemia.
Here's a quick look at some types:
Type | Genes Inherited |
|---|---|
Sickle Cell Anemia | HbS from both parents |
Hemoglobin SC Disease | HbS from one, HbC from other |
Sickle Beta-Thalassemia | HbS from one, beta-thalassemia from other |
Each type can cause red blood cells to sickle, but the amount of normal hemoglobin produced can vary, affecting how severe the symptoms might be. For some individuals with severe forms of SCD, advanced treatments like gene therapy are becoming an option, offering a potential path toward a cure. You can learn more about gene therapy options for sickle cell disease.
Recognizing the Symptoms of Sickle Cell Disease
Sickle cell disease can show up in different ways, and it's not always the same for everyone. The main thing to know is that the red blood cells, which are normally round and flexible, change shape. They become stiff and can look like a crescent moon or a 'C'. This change is what gives the disease its name and causes a lot of the problems.
Common Symptoms and Their Causes
These sickle-shaped cells don't move through the body's blood vessels as smoothly as round ones. They can get stuck and block blood flow. When this happens, it can cause a lot of pain and damage to organs over time. Because these cells also break apart more easily, people with sickle cell disease often have fewer red blood cells than they should. This is called anemia, and it can make you feel really tired and weak.
Pain: This is often the most noticeable symptom. It happens when blood flow is blocked. The pain can show up anywhere in the body, like in the chest, arms, legs, or belly. It can last for a few hours or even a few days.
Anemia: This leads to fatigue, paleness, and sometimes shortness of breath because the body isn't getting enough oxygen.
Jaundice: Sometimes, the skin and the whites of the eyes can look yellow. This happens when the body has trouble processing a substance called bilirubin, which is a byproduct of red blood cells breaking down.
Pain Crises and Their Impact
Pain crises are a big part of living with sickle cell disease. They can be quite severe and often require medical attention. The pain happens when those stiff, sickle-shaped cells clump together and block blood flow in small vessels. This blockage stops oxygen from reaching certain parts of the body, causing intense pain and sometimes swelling.
The unpredictability of pain crises can be really tough. One day might be fine, and the next could bring on a severe episode that lands you in the hospital. It affects daily life, work, and school.
Symptoms in Children
Kids with sickle cell disease can have the same symptoms as adults, but they might also show up a bit differently. For example, babies might have swelling in their hands and feet, which can be one of the first signs. Children might also grow more slowly than other kids their age. It's important for them to get regular check-ups to monitor their growth and catch any problems early. Early diagnosis and care are key for children with sickle cell disease.
Here's a quick look at some common signs in children:
Swelling in hands and feet (dactylitis)
Delayed growth and development
Frequent infections
Episodes of pain
Anemia (leading to tiredness)
Potential Complications of Sickle Cell Disease
Sickle cell disease (SCD) can lead to a number of health problems because the sickle-shaped red blood cells don't move smoothly through the body. These cells can get stuck and block blood flow. This blockage can cause pain and damage to different parts of the body over time. It's important to know about these potential issues so you can work with your doctor to prevent or manage them.
Vaso-Occlusive Crises and Organ Damage
Vaso-occlusive (VO) crises are a hallmark of SCD. This is when those sickle-shaped cells clump together and block small blood vessels. Think of it like a traffic jam in your blood vessels. This blockage stops oxygen-rich blood from reaching certain areas, which can cause a lot of pain, often in the bones, chest, and abdomen. These crises can happen suddenly and can last for hours or even days. Repeated blockages can also lead to damage in organs like the spleen, kidneys, liver, and lungs. The spleen is especially vulnerable, and damage to it can make it harder for the body to fight off infections.
Risk of Stroke and Acute Chest Syndrome
When blood flow to the brain is blocked by sickle cells, it can cause a stroke. In children, this is a serious concern, and sometimes strokes don't have obvious symptoms but can still affect brain development. Signs of a stroke can include sudden weakness, trouble speaking, or seizures. Acute Chest Syndrome (ACS) is another serious complication, particularly affecting the lungs. It can happen when sickle cells block blood flow in the lungs, leading to chest pain, fever, and difficulty breathing. ACS needs immediate medical attention because it can be life-threatening.
Other Health Concerns
Beyond crises and major events like strokes, SCD can cause a range of other issues. These include:
Anemia: Because sickle cells break down faster than normal red blood cells, people with SCD often have chronic anemia, which can lead to fatigue and weakness.
Infections: Damage to the spleen and a weakened immune system make individuals with SCD more prone to infections, some of which can be very serious.
Vision Problems: Blockages in the small blood vessels of the eyes can damage the retina, potentially leading to vision loss.
Leg Ulcers: Open sores, especially on the lower legs, can develop due to poor blood flow.
Gallstones: The breakdown of red blood cells can lead to gallstones.
Priapism: This is a painful, prolonged erection that requires urgent medical care to prevent lasting damage.
Managing sickle cell disease involves not just treating the immediate pain but also being proactive about preventing these long-term complications. Regular check-ups and open communication with your healthcare team are key to staying as healthy as possible.
It's also worth noting that knowing your sickle cell status is important, especially if you're planning a family. While most people with sickle cell trait live normal lives, understanding your genetic makeup can help with family planning and rare health situations. A simple blood test can determine your status if you're unsure. Sickle cell trait means you carry one gene for sickle cell and one normal gene.
Managing and Treating Sickle Cell Disease
Living with sickle cell disease means there are ways to help manage the symptoms and prevent serious problems. It's not about a magic fix, but more about a steady plan to keep things as good as possible. The main goals are to ease pain, stop infections before they start, and keep your organs working well. A big part of this is working closely with your doctors. They'll help create a plan that's just right for you or your child.
Symptom Management and Prevention
When you have sickle cell disease, pain is a big concern. These painful episodes, often called crises, happen when sickle-shaped cells block blood flow. To help manage pain, doctors might suggest over-the-counter pain relievers for milder pain, or stronger medications if the pain is severe. Staying hydrated is also super important; drinking lots of water can help prevent these blockages. Keeping up with vaccinations is another key step to avoid infections, which can be really dangerous for people with sickle cell disease. For example, the pneumococcal vaccine is recommended to protect against certain types of pneumonia.
Stay Hydrated: Drink plenty of water throughout the day. This helps keep your blood flowing smoothly.
Prevent Infections: Get all recommended vaccines and avoid people who are sick.
Manage Pain: Use prescribed pain relievers and non-drug methods like warm baths or gentle exercise when you're not in crisis.
Avoid Triggers: Try to stay away from things that can make a crisis worse, like extreme temperatures or dehydration.
Medications for Sickle Cell Disease
There are a few medications that can make a real difference. One is called hydroxyurea. It works by increasing the amount of fetal hemoglobin (HbF) in your blood. Fetal hemoglobin is the type of hemoglobin babies have before they are born, and it doesn't sickle. By having more HbF, your red blood cells are less likely to change shape, which can mean fewer pain crises and fewer trips to the hospital. It's important to take hydroxyurea regularly as prescribed and to have regular blood tests to check how it's working and to monitor for any side effects. Another medication, L-glutamine, is also used to help reduce complications. For certain situations, like severe anemia or acute chest syndrome, blood transfusions might be needed. These transfusions provide healthy red blood cells to help carry oxygen better and reduce the number of sickled cells in the body. You can learn more about sickle cell disease at the National Heart, Lung, and Blood Institute.
Advanced Treatment Options
For some people with severe sickle cell disease, more intensive treatments might be an option. One of these is a bone marrow or stem cell transplant. This procedure replaces the bone marrow that's making abnormal red blood cells with healthy bone marrow from a donor. It's a complex treatment with potential risks, but it can be a cure for some individuals. Doctors carefully consider who is a good candidate for this type of treatment. There are also ongoing research efforts looking into new medications and therapies that could offer even more ways to manage sickle cell disease in the future.
Diagnosis and Ongoing Care
Diagnostic Testing for Sickle Cell Disease
Figuring out if someone has sickle cell disease (SCD) usually starts with a blood test. The most common test is called hemoglobin electrophoresis. It's like a special way to look at the different types of hemoglobin in your red blood cells. People with SCD have a different kind of hemoglobin, called hemoglobin S, which makes their red blood cells stiff and shaped like a sickle, or crescent moon. This test can tell us if someone has SCD or if they carry the sickle cell trait (meaning they have one gene for normal hemoglobin and one for sickle cell hemoglobin).
For newborns, SCD is often found through routine screening tests done shortly after birth. This is super important because catching it early means we can start managing it right away to help prevent problems. If a newborn screening shows something, more tests will be done to be sure.
Sometimes, other tests might be needed to see how SCD is affecting different parts of the body. This could include things like:
Ultrasound: To look at organs like the spleen or kidneys.
MRI: To get detailed pictures of organs and check for any damage.
Transcranial Doppler ultrasound: This is a special test to check blood flow in the brain and see if there's a higher risk of stroke.
Importance of Regular Medical Care
Living with sickle cell disease means you'll need to see your doctor regularly. It's not a one-time fix; it's something that needs ongoing attention. Think of it like keeping up with regular check-ups for your car to make sure it runs smoothly. For SCD, these regular visits are key to staying as healthy as possible.
During these appointments, your healthcare team will:
Monitor your health: They'll check your blood counts, look for any signs of complications, and make sure any treatments you're on are working well.
Prevent problems: They'll talk about ways to avoid things that can trigger pain crises or other issues, like staying hydrated and getting vaccinated.
Manage symptoms: If you're having pain or other symptoms, they'll work with you to find the best ways to manage them.
Adjust treatments: As you grow or if your condition changes, your treatment plan might need to be updated.
It's also really helpful to have a team that understands SCD well. This might include doctors, nurses, social workers, and other specialists who can help with all the different aspects of living with the condition. They can provide support, education, and resources for you and your family.
Having a strong relationship with your healthcare providers is a big part of managing sickle cell disease effectively. Don't hesitate to ask questions or share any concerns you have. They are there to help you navigate life with SCD.
These regular check-ins and a good care team make a big difference in managing SCD and helping people live fuller lives.
Navigating the path after a diagnosis and during ongoing care can feel overwhelming. Many families face tough choices about treatments like gene therapy, often with many questions about what comes next. We're here to help you understand all your options and provide support every step of the way. Visit our website to learn more about how we can help your family.
Wrapping Up Our Talk on Sickle Cell Disease
So, we've gone over what sickle cell disease is all about – how it's passed down, what happens to red blood cells, and the kinds of issues it can cause, like pain and fatigue. We also touched on how doctors manage it, from medicines to more involved treatments. It's a lot to take in, for sure. Knowing the basics helps everyone, whether you have it, care for someone who does, or are just curious. It's a condition that needs attention and understanding, and hopefully, this has shed some light on it.
Frequently Asked Questions
What exactly is sickle cell disease?
Sickle cell disease, often called SCD, is a sickness you're born with that affects your red blood cells. Normally, red blood cells are round and flexible, like tiny donuts, helping them travel easily through your body to deliver oxygen. But with SCD, some of these cells become stiff and shaped like a crescent moon or a sickle. These sickle-shaped cells can get stuck and block blood flow, causing pain and other health problems.
What makes red blood cells sickle-shaped?
It all starts with a tiny change, called a mutation, in the instructions (genes) that tell your body how to make hemoglobin. Hemoglobin is the part of your red blood cells that carries oxygen. In sickle cell disease, this gene change causes the body to make an abnormal type of hemoglobin, known as hemoglobin S. When there isn't enough oxygen, this hemoglobin S makes the red blood cells stiff and turn into that sickle shape.
How do people get sickle cell disease?
Sickle cell disease is inherited, meaning it's passed down from parents to children through genes. To have sickle cell disease, a person needs to inherit two copies of the sickle cell gene, one from each parent. If someone only gets one copy, they are a carrier and usually don't have symptoms, but they can still pass the gene on.
What are the main signs of sickle cell disease?
One of the most common and difficult symptoms is severe pain, often called a pain crisis. This happens when the sickle-shaped cells block blood flow. People with SCD can also feel very tired because they have fewer red blood cells (anemia), and they might get infections more easily. Sometimes, the skin and eyes can look yellow, a condition called jaundice.
Can sickle cell disease cause other health issues?
Yes, unfortunately. The blocked blood flow from sickle cells can damage organs over time, like the spleen, kidneys, and lungs. It also increases the risk of serious problems such as stroke, which happens when blood flow to the brain is blocked, and acute chest syndrome, a dangerous lung complication. Swelling in the hands and feet is also common, especially in children.
What can be done to help people with sickle cell disease?
There are several ways to manage sickle cell disease. Doctors focus on relieving pain during crises, preventing infections with medicines and vaccines, and making sure the body gets enough oxygen, sometimes through blood transfusions. There are also special medicines, like hydroxyurea, that can help reduce the number of pain crises. For some people with severe SCD, a bone marrow or stem cell transplant might be an option to cure the disease.
.png)


Comments